World Suicide Prevention Day (WSPD), marked each year on 10 September, is organized by the International Association for Suicide Prevention (IASP) in conjunction with the World Health Organization (WHO). The purpose of this day is to raise awareness around the globe that suicide can be prevented.
It highlights the importance of addressing suicide and mental health issues globally. In Tanzania, this day brings to the forefront the increasing recognition of mental health and suicide as critical public health challenges, particularly in the face of cultural stigma and limited resources.
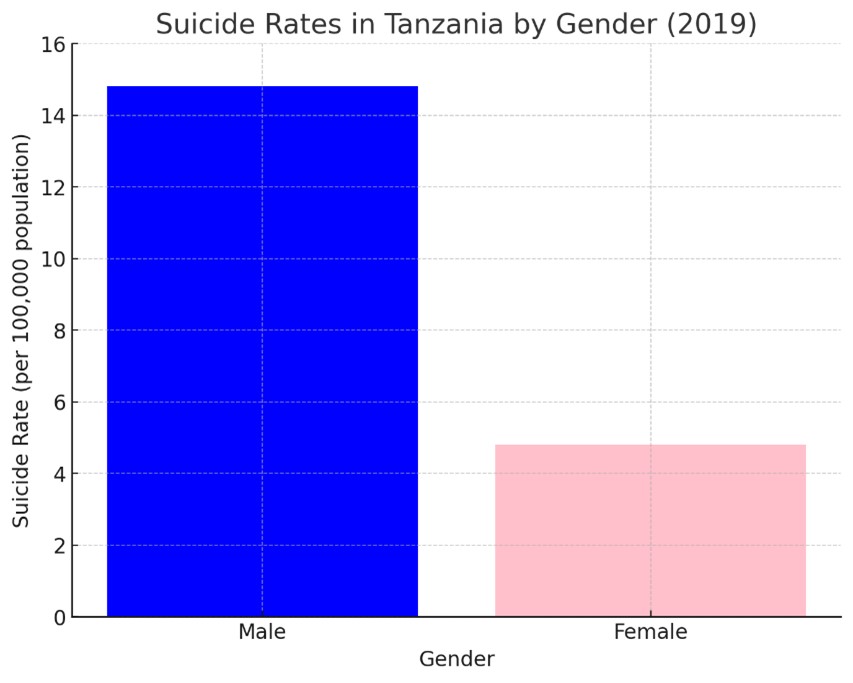
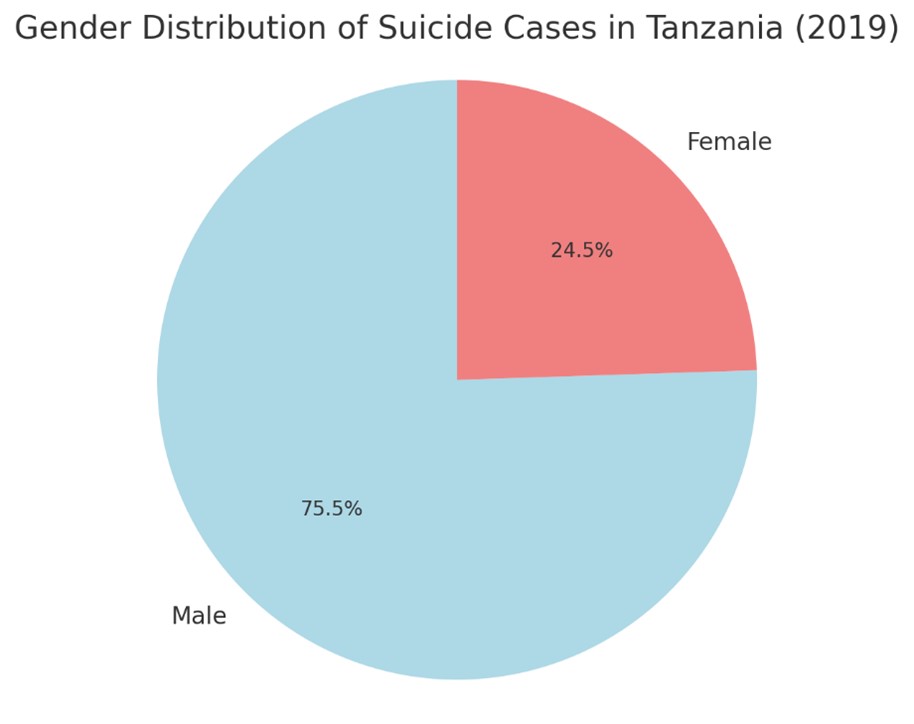
World Health Organization (WHO) highlights in Tanzania a stark gender disparity in 2019, with males having a suicide rate of 14.8 per 100,000, over three times higher than the female rate of 4.8 per 100,000. This emphasizes the need for targeted mental health interventions addressing the specific challenges faced by men in Tanzania.
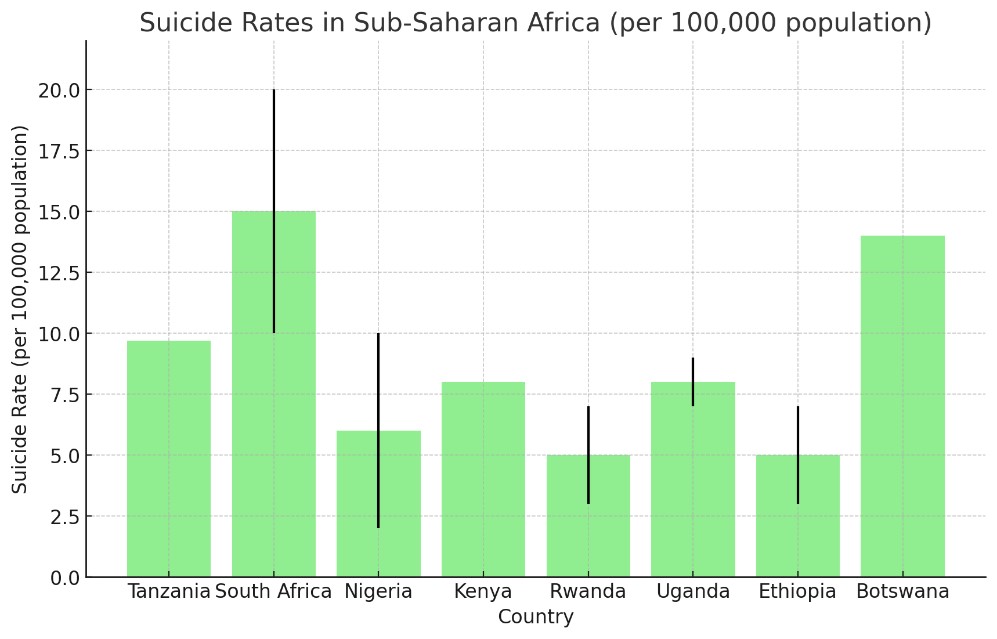
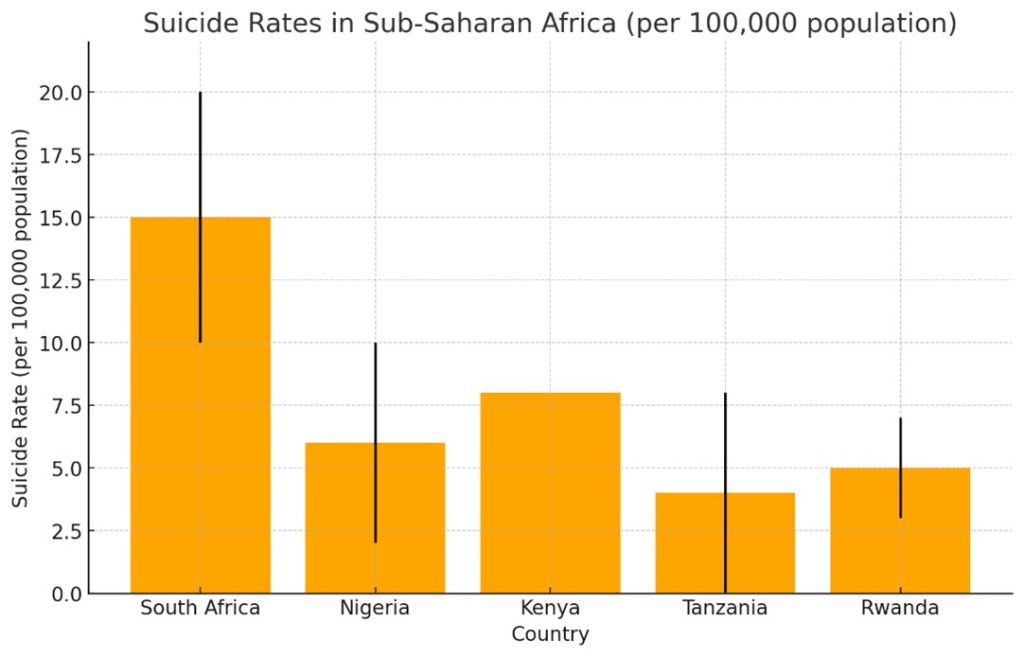
In the same report, the World Health Organization (WHO) highlighted significant variations in suicide rates across Sub-Saharan Africa. South Africa had the highest rate, ranging from 15 to 20 per 100,000, followed by Botswana at 14 per 100,000. Tanzania’s rate was 9.7 per 100,000, Uganda’s was 8 to 9 per 100,000, and Kenya’s was 8 per 100,000.
Nigeria’s rate varied between 6 and 10 per 100,000, while Rwanda and Ethiopia had lower rates of 5 to 7 per 100,000. These disparities point to diverse mental health challenges, with South Africa and Botswana facing the most critical issues.
The report also shows that 75.5% of suicide cases involved males, while 24.5% involved females. This significant disparity indicates that men are disproportionately affected by suicide in Tanzania, with males accounting for more than three-quarters of the total cases. This highlights the need for targeted mental health interventions, particularly focused on addressing the factors contributing to higher suicide rates among men.
READ RELATED: Mental Health Matters: Empowering Tanzania’s Well-Being Revolution
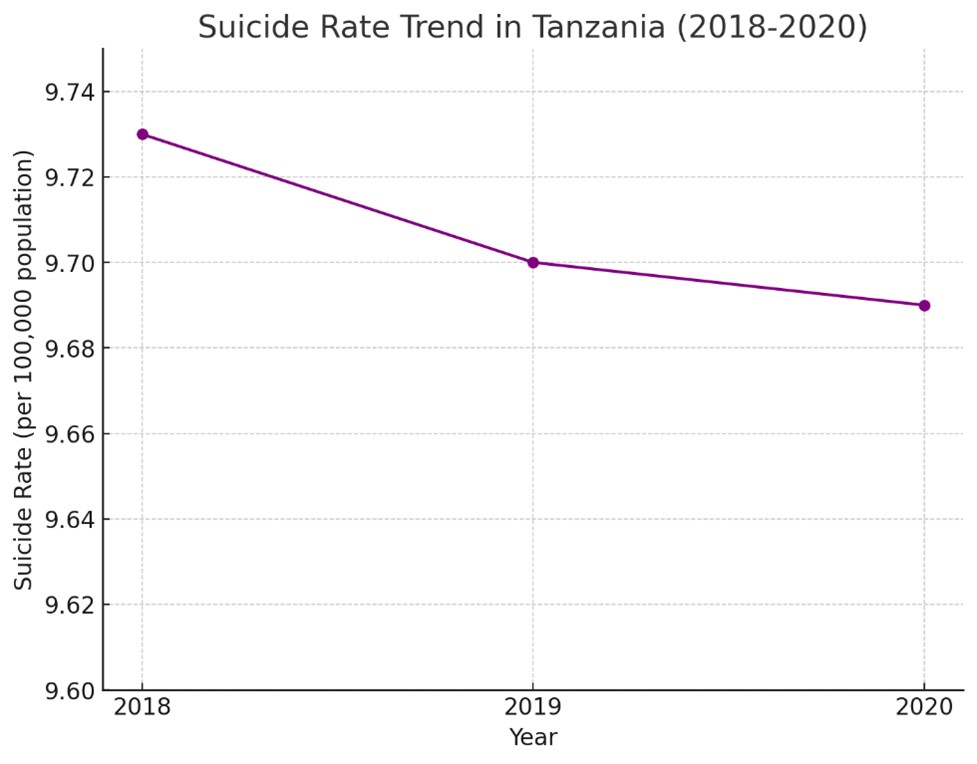
The report illustrates a slight decline in suicide rates over the three-year period. In 2018, the rate was approximately 9.73 per 100,000, which decreased to 9.70 in 2019 and further to 9.69 in 2020.
Although the decrease is gradual, it indicates a minor improvement in suicide prevention efforts. However, the trend emphasizes the need for sustained efforts in mental health awareness and interventions to continue reducing suicide rates in Tanzania.
Research Findings
Mental health research in Tanzania paints a concerning picture, especially in rural areas where services are scarce. The 2021 study “Suicide in Tanzania” estimates rates between 4 to 8 per 100,000, with the situation worsening in underserved regions.
Cultural stigma and underreporting, as revealed in the 2020 study “Mental Health and Stigma,” continue to hold back public awareness. Even more troubling, the 2019 study “Assessing Mental Health Services” highlights severe shortages in professionals and facilities, while the 2022 study “Cultural Influences on Mental Health” shows stigma still prevents many from seeking help.
Despite efforts from governments and NGOs, underserved areas remain difficult to reach. The 2024 study “Strategic Recommendations” pushes for urgent action—better data collection, more services, and stronger public education to tackle these pressing mental health challenges.
These findings collectively underscore the importance of addressing mental health and suicide issues in Tanzania through enhanced awareness, resource allocation, and support systems.
These findings collectively underscore the importance of addressing mental health and suicide issues in Tanzania through enhanced awareness, resource allocation, and support systems.
Happenings
In Dodoma, on the afternoon of May 16, 2024, tragedy struck when Bishop Joseph Bundala, 55, of the Methodist Church, took his own life in his office. Struggling with overwhelming debts, he used a telephone wire to end his life, leaving the community in shock.
Similarly, in Sinza, Dar es Salaam, the residents were left in disbelief in late July 2021 when 29-year-old accountant Alex Korosso, consumed by personal turmoil, shot his friend during a heated argument over drinks and then turned the gun on himself.
In Mwanza, Jorum Makumbi continues to be haunted by the memory of a phone call delivering the devastating news of his 21-year-old son Bakari’s suicide. “It’s a trauma I can hardly bear to remember,” Makumbi says, reflecting on the mystery surrounding Bakari’s decision to hang himself with a bedsheet.
Meanwhile, Mary Lyatuu endures a daily struggle with grief. Every evening, she visits her daughter Sarah’s grave at Kinondoni Cemetery in Dar es Salaam, seeking solace in prayer. Sarah, despite her academic achievements, was unable to find a job, leading her into deep despair and, tragically, to take her own life in early 2021.
Statistics
Suicide rate data in Sub-Saharan Africa is limited due to data collection challenges and varying healthcare infrastructure, as seen from estimates that differ from WHO findings. The Global Burden of Disease (GBD) study estimates an age-standardized rate of about 7 per 100,000, with rising trends in some areas.
For instance, South Africa’s suicide rate is 15 to 20 per 100,000, Nigeria’s ranges from 6 to 10, and Kenya’s is around 8. In Tanzania, the rate varies between 4 to 8 per 100,000, though underreporting and stigma make the data unreliable.
Despite progress in mental health integration, such as Rwanda’s efforts to include it in primary care, challenges remain. Effective prevention in the region requires improved national policies, greater awareness, and enhanced mental health services.
Way Forward
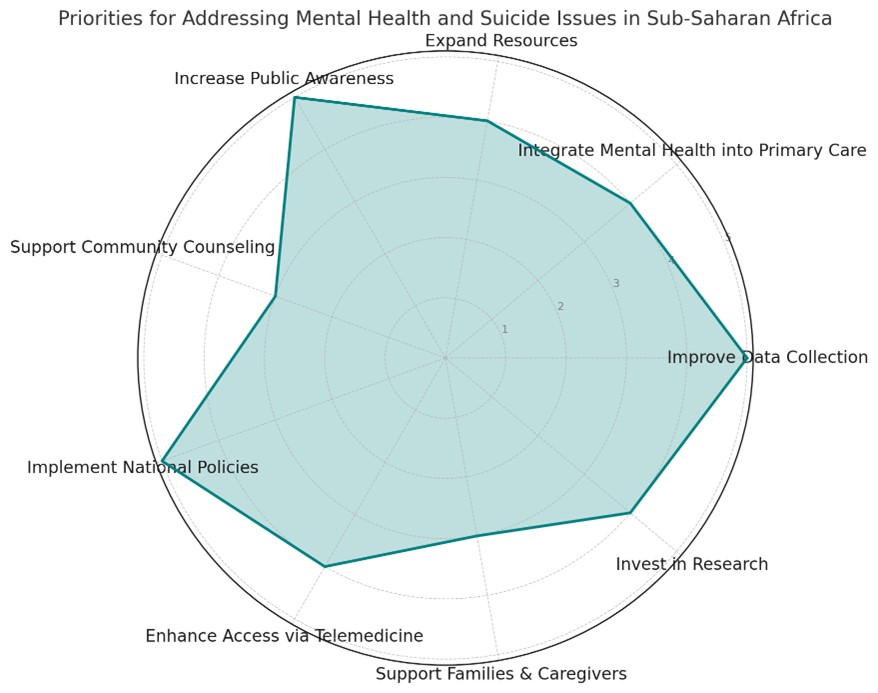
To address mental health and suicide issues in Sub-Saharan Africa, including Tanzania, emphasis on key areas for intervention, such as improving data collection, increasing public awareness to reduce stigma, and integrating mental health into primary care.
Expanding resources, supporting community counseling, and implementing strong national policies with suicide prevention strategies are also critical.
Additionally, enhancing telemedicine access, supporting families, and investing in research are vital for long-term progress. The chart highlights public awareness, data collection, and policy implementation as foundational priorities for effective mental health interventions.
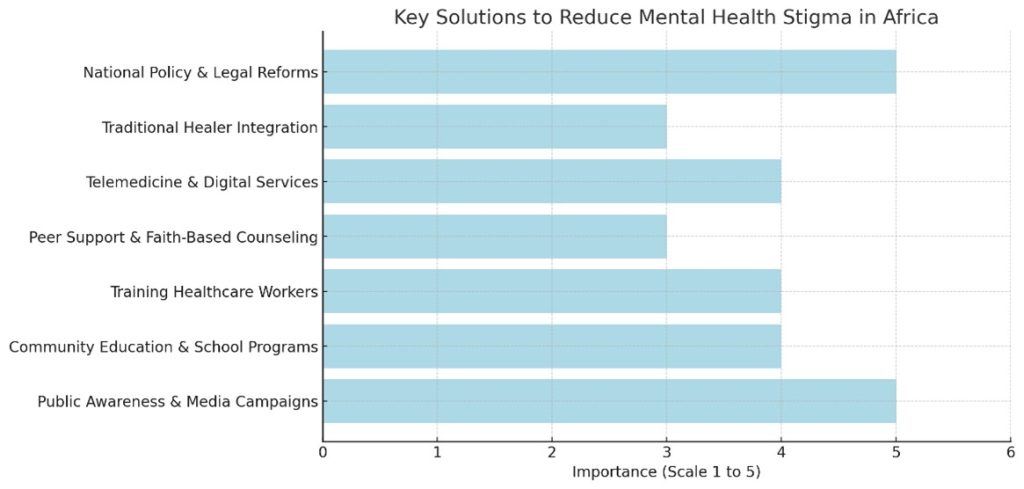
Reducing mental health stigma in Africa requires raising public awareness, educating communities, and integrating mental health services into primary care. Public campaigns, school programs, and media initiatives can dispel myths about mental illness. Training healthcare workers and involving community leaders help spread accurate information.
Peer support groups, faith-based counseling, and accessible telemedicine services can also encourage people to seek help. Collaborative efforts between traditional healers and modern healthcare providers ensure cultural sensitivity. Strengthening national policies and increasing research further supports mental health initiatives in the region.
Former Health Minister Hon. Ummy Mwalimu urged health stakeholders to prioritize preventive measures in tackling mental health challenges, highlighting the rising number of affected individuals.
Citing international statistics, she emphasized that one in every eight people globally faces a mental health issue, and in Tanzania alone, an estimated seven million people are living with various mental health conditions, many of which are linked to drug abuse.